You check your blood pressure at your annual physical. Your doctor nods approvingly. Your cholesterol numbers? “Within range”. Exercise? You're doing your best to stay active. By all conventional measures, your heart health looks fine.
Yet we routinely see patients with "normal" cholesterol and acceptable blood pressure who are already showing early signs of metabolic strain, rising triglycerides, creeping fasting insulin, subtle glucose variability that never appears on a standard lab report.
Long before LDL climbs or plaque becomes visible on imaging, the body's fuel regulation system begins to lose flexibility. This is metabolic flexibility, your body's ability to switch between burning glucose and fat efficiently, and it may be one of the most important drivers of cardiovascular resilience that rarely gets discussed in routine care.
What Is Metabolic Flexibility?
Metabolic flexibility is your body's capacity to seamlessly switch between burning glucose and fat for energy, depending on what's available and what you're doing. Think of it as your metabolism's ability to shift gears, like a hybrid car that knows when to use gas and when to tap into its electric battery.
When you're metabolically flexible, your body responds appropriately to different situations. After a meal, it efficiently uses the incoming glucose. Between meals or during exercise, it smoothly transitions to burning stored fat. Your cells are responsive, adaptable, and resilient.
When you're metabolically inflexible, a state that often accompanies insulin resistance, your body gets stuck in sugar-burning mode. Your cells struggle to access fat stores for energy. You experience energy crashes, persistent cravings, and difficulty maintaining stable blood sugar. This metabolic rigidity sets off a cascade of changes that directly impact your cardiovascular system.
How Blood Sugar Dysregulation Harms Your Heart
The relationship between blood sugar management and heart health runs far deeper than most people realize. It's not just about diabetes or prediabetes. Even subtle blood sugar dysregulation creates a perfect storm for cardiovascular damage.
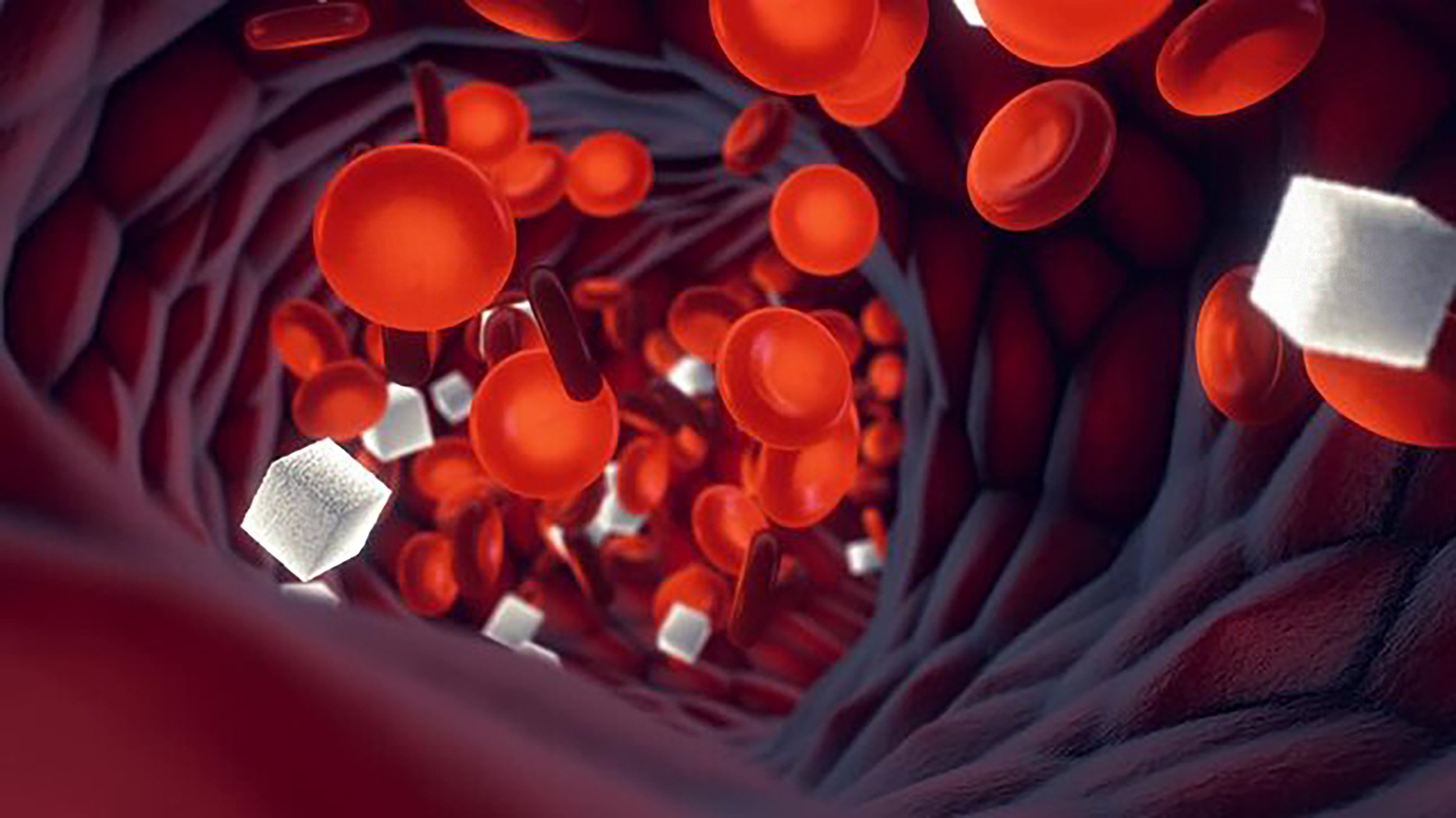
Endothelial Dysfunction: Your endothelium is the delicate inner lining of your blood vessels. When blood sugar spikes repeatedly throughout the day, it triggers oxidative stress and inflammation that damage this crucial layer. Studies show that postprandial glucose spikes are particularly damaging, generating more oxidative stress than chronically elevated blood sugar.
Advanced Glycation End Products (AGEs): When excess glucose circulates in your bloodstream, it binds to proteins through glycation, forming harmful compounds called AGEs. These sticky molecules accumulate in blood vessel walls, making them stiff and dysfunctional. They trigger inflammation and accelerate atherosclerosis. Controlling blood sugar excursions dramatically reduces new AGE formation.
Chronic Inflammation: Metabolic inflexibility fuels chronic, low-grade inflammation, "metabolic inflammation" that damages tissues over time. Elevated blood sugar activates inflammatory pathways and reduces the body's anti-inflammatory capacity. This chronic inflammatory state drives atherosclerosis and cardiovascular events.
Insulin Resistance and Blood Pressure: Insulin resistance doesn't just affect blood sugar, it directly impacts blood pressure through increased sodium retention, activation of the sympathetic nervous system, and impaired blood vessel relaxation. Many people don't realize their blood pressure struggles are rooted in metabolic dysfunction.
Dyslipidemia: Metabolic inflexibility creates a characteristic lipid pattern: elevated triglycerides, low HDL cholesterol, and small, dense LDL particles that are particularly atherogenic. This metabolic dyslipidemia is driven by insulin resistance and poor blood sugar control.
Clinical Pattern Recognition
One of the most common patterns we see isn't overt diabetes. It's high-functioning adults with fasting glucose in the "normal" range but fasting insulin quietly elevated. Triglycerides inch upward. HDL drifts lower. Blood pressure creeps from 112/70 to 128/82 over a few years.
Individually, none of these numbers trigger alarm. Collectively, they reflect a metabolism losing flexibility. This is not sudden heart disease. It's gradual metabolic rigidity that often develops years before conventional thresholds are crossed.
Early Warning Signs
Physical symptoms include energy crashes 2-3 hours after meals, intense carbohydrate cravings, difficulty fasting, brain fog between meals, trouble losing weight, and frequent hunger even after eating.
Early metabolic markers to watch include fasting insulin above 6 μIU/mL, hemoglobin A1c trending above 5.2–5.3%, triglycerides above 80 mg/dL, a triglyceride-to-HDL ratio above 2:1, and fasting glucose consistently above 85 mg/dL.
Cardiovascular clues include blood pressure trending upward, increasing waist circumference, skin tags, family history of early heart disease, and elevated inflammatory markers.
Building Metabolic Flexibility: Your Roadmap
The extraordinary news is that metabolic flexibility can be restored. Here's how functional medicine approaches this transformation.
Dietary Strategies: Focus on blood sugar-stabilizing meals combining quality protein, healthy fats, and fiber with moderate complex carbohydrates. Optimize meal timing by front-loading carbohydrates earlier in the day when insulin sensitivity is naturally higher. Consider extending your overnight fast to 12-14 hours. Prioritize whole, minimally processed foods.
Exercise: Both resistance training and aerobic exercise improve insulin sensitivity. Strength training increases muscle mass, which serves as a metabolic sink for glucose disposal. Zone 2 cardio, moderate-intensity aerobic exercise, specifically trains your body to efficiently burn fat. High-intensity interval training provides complementary benefits. Consistency and variety are key.
Sleep: Poor sleep powerfully drives insulin resistance. A single night of sleep deprivation can reduce insulin sensitivity by up to 30%. Prioritize 7-9 hours of quality sleep and address sleep disorders like sleep apnea.
Stress Management: Chronic stress keeps cortisol elevated, which raises blood sugar and promotes insulin resistance. Incorporate stress-reduction practices: meditation, breathwork, yoga, time in nature, or creative activities.
Targeted Supplementation: While food and lifestyle form the foundation, certain supplements can support metabolic flexibility including berberine, omega-3 fatty acids, magnesium, alpha-lipoic acid, chromium, and cinnamon. Supplementation should be personalized based on individual needs.
Addressing Root Causes: Functional medicine recognizes that metabolic inflexibility doesn't occur in isolation. We assess gut health, chronic infections, toxin exposure, hormonal imbalances, and genetic factors.
Time-Restricted Eating: One of the most effective strategies is limiting your food intake to a specific window each day, typically 8-12 hours. During fasting periods, your body exhausts readily available glucose and begins accessing fat stores. This regular practice strengthens your ability to transition between fuel sources and improves insulin sensitivity.
The Functional Medicine Advantage
At CCFM, we look for patterns long before disease is diagnosed, utilizing our proprietary VitOS™ Index to interpret functional markers through the lens of resilience, adaptability, and long-term cardiovascular health.
Our comprehensive approach goes beyond standard lab panels to include advanced diagnostic testing, continuous glucose monitoring for real-time metabolic insight, personalized nutrition and lifestyle strategies, targeted supplementation, and ongoing clinical guidance. The goal isn’t simply to prevent disease, it’s to build a cardiovascular system that remains flexible, responsive, and strong for decades.
Designing Your Cardiovascular Future
Metabolic flexibility isn't just about blood sugar. It's about whether your cardiovascular system stays adaptive or gradually becomes rigid. Resilient systems respond appropriately to stress, recover efficiently, and adjust. Rigid systems struggle, overcorrect, inflame, and stiffen.
The good news is that metabolic flexibility can be restored. The same strategies that improve glucose regulation also reduce inflammation, improve lipid quality, support vascular function, and enhance energy.
You don't need a diagnosis of diabetes or heart disease to begin paying attention. The most powerful interventions happen before those diagnoses ever appear. Your cardiovascular future is written in how adaptable your metabolism remains over time.
Your heart's future is shaped by choices you make today. Make them count.