You go in for your annual physical. Your cholesterol is checked. Your doctor says, "Looks fine."
You leave reassured.
But most cardiovascular disease doesn't begin with a dramatic cholesterol spike. It develops quietly, often years before anything falls outside the conventional "normal" range.
The Problem With "Normal"
Conventional lab ranges are designed to detect disease, not identify risk early.
Consider these examples:
- An A1c of 5.6% is considered normal but our VitOS™ Index identifies optimal function at 4.6-5.3%
- A triglyceride level of 140 mg/dL may not raise alarm, yet optimal metabolic health shows triglycerides between 40-80 mg/dL
- An LDL of 110 mg/dL may get a casual "we'll monitor it", while functional optimization targets levels below 70 mg/dL
None of those values trigger medication. But all of them may signal metabolic strain.
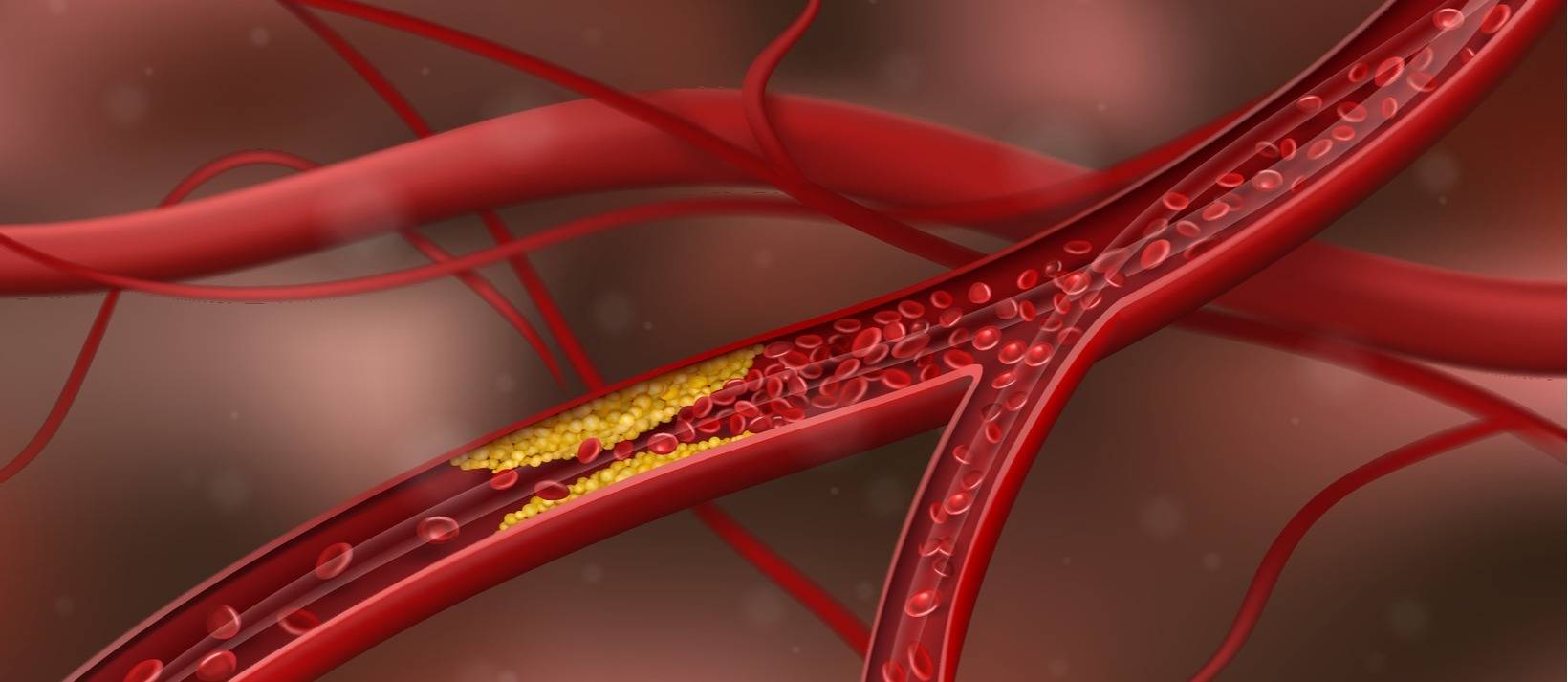
Cholesterol Is Only One Piece of the Puzzle
Cholesterol travels in particles through an environment shaped by insulin, inflammation, liver function, thyroid activity, nutrient status, and genetic risk.
When that environment is unhealthy, even moderate cholesterol levels can become problematic. When it's resilient, the same numbers look very different.
This is why we rarely look at LDL in isolation.
The Markers That Change the Conversation
1. Insulin: The Early Driver
One of the strongest predictors of cardiovascular disease isn't LDL, it's insulin.
Many patients have fasting insulin levels that are technically "normal" but functionally elevated. Using our VitOS™ Index, we target fasting insulin below 6 μIU/mL, a threshold that reflects optimal metabolic function rather than simply the absence of disease. Over time, chronically elevated insulin:
- Increases triglycerides
- Suppresses HDL
- Drives arterial inflammation
- Promotes endothelial dysfunction
By the time glucose or A1c rise significantly, insulin resistance has often been developing for years. We look for optimal insulin patterns long before diabetes is on the table.
2. ApoB: Particle Number Matters More Than Cholesterol Content
Two people can have the same LDL-C. One may have relatively few cholesterol particles. The other may have many small, dense particles.
ApoB measures the number of atherogenic particles and often reveals risk that LDL alone misses. In our VitOS™ Index, we aim for ApoB below 70 mg/dL, a level associated with significantly reduced cardiovascular events. It's one of the most important markers most people have never heard of.
3. Lp(a): The Genetic Wildcard
Lp(a) is largely genetic and significantly elevates lifetime cardiovascular risk. It's not part of a standard lipid panel.
If you've never had it measured, you may be missing a critical piece of your risk profile especially if heart disease runs in your family. The VitOS™ Index sets optimal Lp(a) below 30 mg/dL (or below 50 nmol/L), with elevated risk beginning above 50 mg/dL.
4. Inflammation: The Silent Accelerator
Cardiovascular disease is fundamentally inflammatory.
High-sensitivity CRP (hs-CRP) is one of the simplest ways to assess systemic inflammation. A value of 2 mg/L may be labeled "normal," but functionally, it may represent an inflammatory environment where arterial plaque becomes more unstable. We target hs-CRP below 1 mg/L in the VitOS™ Index, a level where inflammation is truly minimal.
Cholesterol builds the structure. Inflammation destabilizes it.
5. Liver and Metabolic Health
Markers like ALT, AST, and GGT are often viewed as "liver tests." But mild elevations can signal metabolic stress, fatty liver tendencies, and oxidative strain, all of which directly influence cardiovascular risk.
The liver regulates lipid metabolism. When it's under strain, the entire cardiovascular picture shifts.
A Different Way to Think About Risk
Instead of asking whether a lab result is normal, we're looking at the bigger picture:
- Is blood sugar tightly regulated?
- Is inflammation low?
- Is particle burden minimal?
- Is the liver functioning optimally?
- Is the thyroid supporting metabolic balance?
- Are nutrient levels supporting vascular repair?
We organize these markers into our VitOS™ Index—structured optimal ranges, not just normal versus abnormal—to identify where physiology is thriving and where it may be drifting.
This allows us to detect:
- Early insulin resistance
- Subclinical inflammation
- Particle risk not reflected in LDL alone
- Metabolic stress long before diagnosis
It shifts the conversation from disease treatment to proactive resilience.
Clarity Before Crisis
Heart disease doesn't usually arrive suddenly. It develops gradually through metabolic inflexibility, low-grade inflammation, hormonal shifts, and vascular dysfunction.
These changes are often detectable, sometimes decades, before a cardiac event.
The goal isn't to create fear. It's to create clarity.
When you understand your physiology at this level, interventions become targeted and strategic instead of reactive.
One Marker Never Tells the Full Story
If you've been told your cholesterol is "fine" but you still feel uncertain about your long-term health, trust that instinct.
Cardiovascular risk is more nuanced than a single LDL number.
At CCFM, we evaluate cardiac health as a systems issue, not a single marker problem.
Cholesterol definitely matters. It's just not the whole story.